ABSTRACT
Malignant melanoma has a high propensity for cardiac metastasis, with autopsy studies reporting an incidence of 47-64%. However, in living patients, Cardiac Metastases of Malignant Melanoma (CMMM) are rare (<2%) and often diagnosed postmortem. A 46-year-old woman was presented with dyspnea and fatigue. Sixteen years earlier, she had undergone treatment for malignant melanoma of the right forearm. Echocardiography revealed a right atrial mass (6.5×3.7 cm) intermittently obstructing the tricuspid valve and a smaller mass in the right atrial appendage. PET imaging showed no systemic metastases. Due to the risk of tricuspid obstruction and embolization, the patient underwent emergency surgical resection. Histopathology confirmed metastatic malignant melanoma. Postoperative recovery was uneventful, and she was discharged on postoperative day 11 to continue oncology-directed therapy. At six-month follow-up, she remained asymptomatic. CMMM can present decades after primary melanoma treatment. Advances in imaging facilitate earlier detection, yet diagnosis remains challenging. Surgical excision is the preferred treatment in symptomatic cases. Despite historically poor prognosis, survival has improved with modern immunotherapy. This case underscores the importance of lifelong melanoma surveillance and timely surgical intervention in cases of cardiac obstruction.
INTRODUCTION
Malignant melanomas are rare but have a high propensity for metastasizing to the heart, with rates between 47% and 64% observed in autopsy series[1,2] Most cases of Cardiac Metastasis from Malignant Melanoma (CMMM) are diagnosed postmortem. However, the incidence of CMMM in living patients with malignant melanoma is less than 2%.[1,3] CMMM can have an unpredictable clinical presentation, ranging from asymptomatic to life-threatening. It may be diagnosed shortly after treatment of the primary melanoma or even decades later. In this report, we present a case of a 46-year-old woman who required emergency surgery due to obstruction of the tricuspid valve by a right atrial mass, 16 years after being diagnosed with malignant melanoma of the right forearm skin.
CASE REPORT
A 46-year-old woman was transferred from an outside hospital with a documented right atrial mass causing intermittent obstruction of the tricuspid valve. Prior to admission, the patient had experienced occasional dyspnea, fatigue, and decreased tolerance for physical exertion lasting at least three months. Her medical history included malignant melanoma of the right forearm, treated 16 years prior, and lung aspergillosis, surgically treated on two occasions (5 and 3 years prior to admission). A chest X-ray showed a normal-sized heart, and an electrocardiogram confirmed normal sinus rhythm (HR=75/min). A transthoracic echocardiogram revealed normal left ventricular systolic function (EF=62%) and an echogenic mass in the right atrium. Transesophageal Echocardiography (TEE) confirmed a mobile mass (6.5 cmx3.7 cm) attached to the right atrial wall, intermittently obstructing the tricuspid valve, along with a smaller fixed mass (2.7 cm x 1.8 cm) in the right atrial appendage [Figure 1a]. The superior and inferior vena cava orifices were free of involvement. Positron Emission Tomography (PET) was performed to assess for other potential metastatic sites, but no additional findings were observed. Coronary angiography revealed no atherosclerotic changes, and the patient was scheduled for emergency heart surgery to prevent complete tricuspid valve occlusion and/or embolic events.
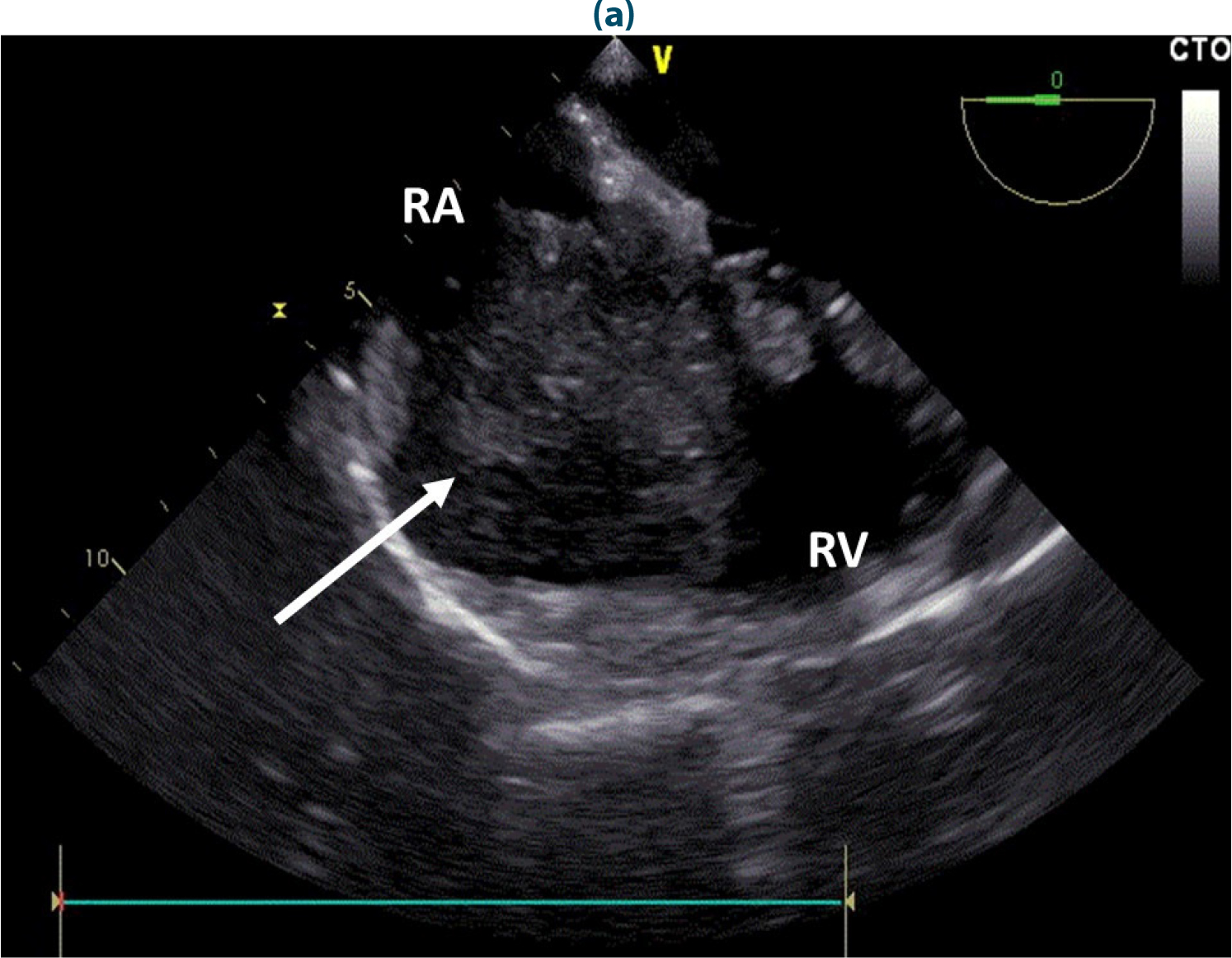
Figure 1:
Intraoperative transesophageal echocardiography showing the right side of the heart (a) before and (b) after surgery. The arrow points to an atypical mass in the right atrium obstructing the tricuspid valve. RA=right atrium; RV=right ventricle.
The heart was cannulated using bicaval venous cannulation, arrested, and an on-pump procedure was performed. Careful surgical manipulation was used to avoid the risk of iatrogenic embolization. Upon right atriotomy, an oval red-brown solid mass was found attached to the free right atrial wall, surrounded by thrombotic material and leaning against the tricuspid valve. Another oval mass was identified in the right atrial appendage. Both masses were completely resected [Figure b], with the tricuspid valve and right atrium left intact.
Gross examination revealed both tumor masses to be solid with uneven surface structures. On cross-section, they appeared mottled, grayish-brown to yellow, partly necrotic, and infiltrated with blood [Figure 2]. Microscopically, the tumor tissue was composed of polygonal atypical melanocytes, with an increased nucleocytoplasmic ratio, hyperchromatic and vesicular nuclei, focal eosinophilic nucleoli, and bright cytoplasm. Numerous pathological mitoses and multinucleated tumor cells were also noted [Figure 3]. Immunohistochemically, the tumor cells were diffusely positive for melanin A, focally positive for HMB45, diffusely positive for S100, and negative for panCK [Figure 4]. Based on the histological appearance and immunohistochemical profile, the diagnosis was confirmed as epithelioid-type malignant metastatic melanoma in the right atrium.

Figure 2:
Gross view of the resected right atrial mass. On cross-section, the tumor is a solid structure, grayish-brown to yellow, partly necrotic and permeated with blood.
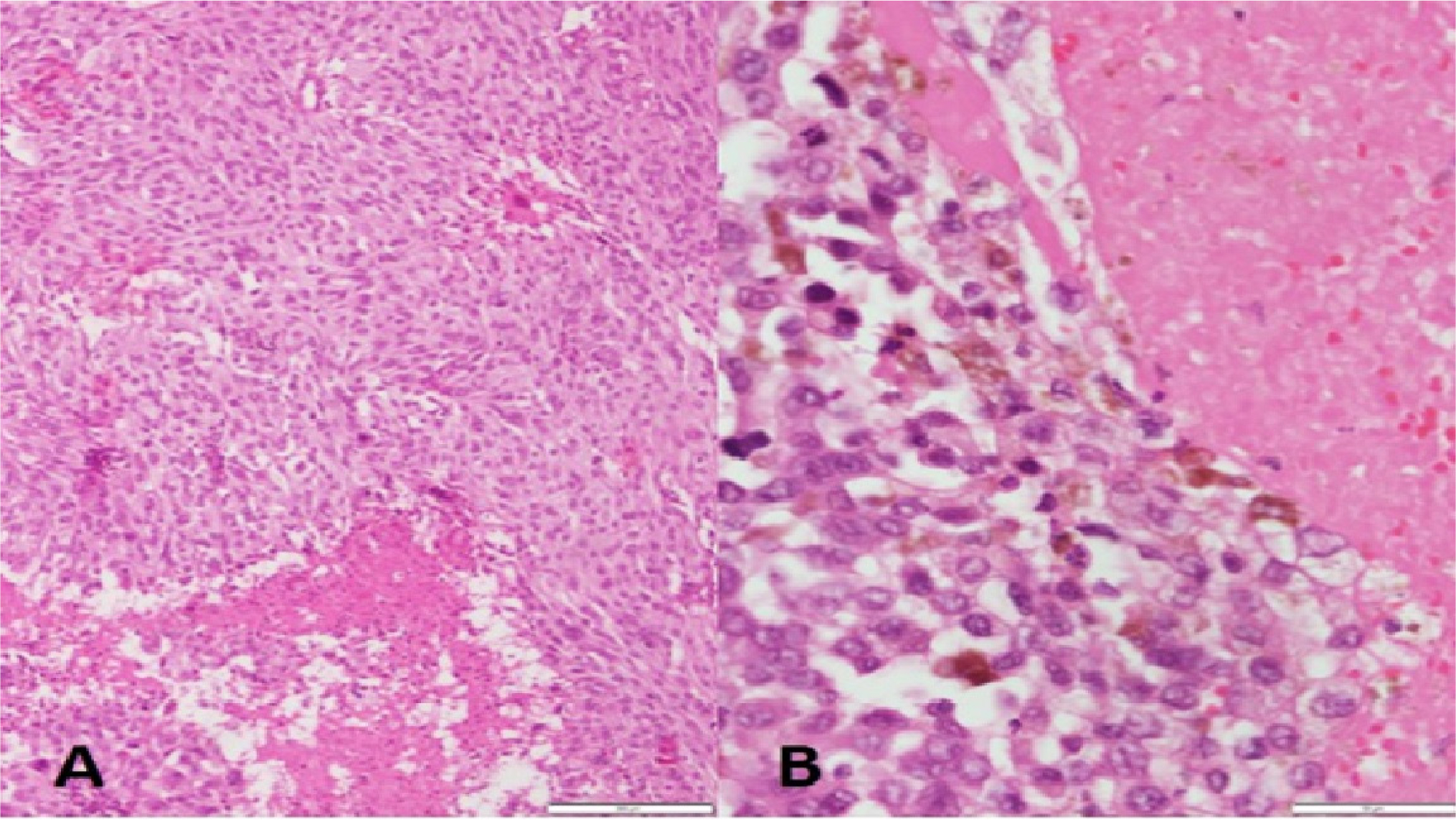
Figure 3:
Histological section of the resected intracardiac malignant melanoma. Tumor shows atypical melanocytes (A) and dense intracytoplasmic melanin pigment (B). Hematoxylin and eosin stain, original magnification 10x (A) and 40x (B).
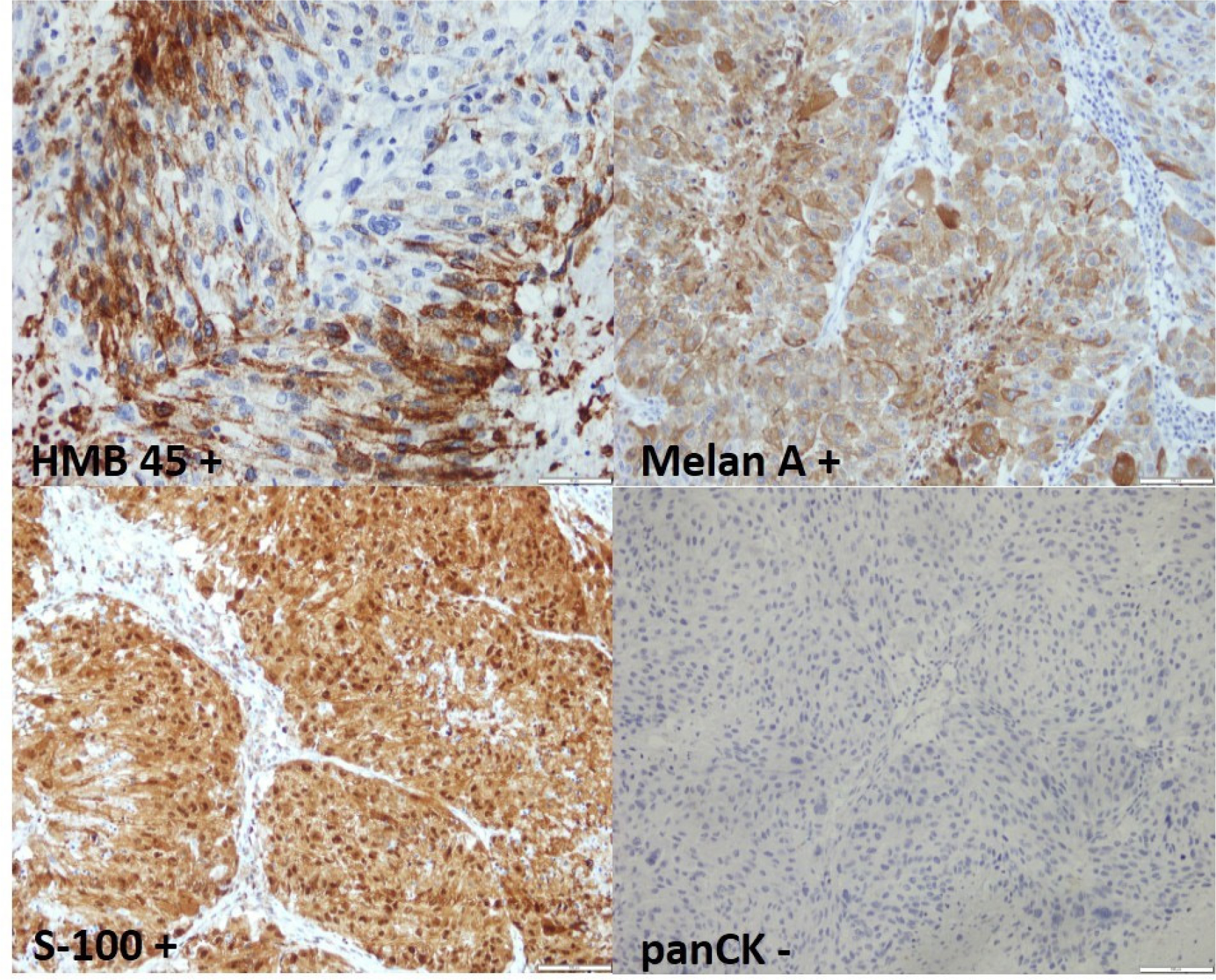
Figure 4:
Immunohistochemistry showing tumor cells positive for HMB45 (40x), melanin A (40x), S-100 (20x), and negative for panCK (20x).
The patient’s postoperative course was uncomplicated, and she was discharged 11 days after surgery to continue oncology treatment. She remained symptom-free and well 6 months later.
DISCUSSION
Malignant melanoma is a highly aggressive neoplasm with widespread potential for metastasis, variable clinical presentations, and unpredictable behavior. It arises from neoplastic changes in melanocytes located in the skin, mucous membranes, gastrointestinal tract, eyes, or meninges.[4] CMMM typically presents as a multifocal pericardial or myocardial mass, rarely involving endocardial cavities. When it does involve the endocardium, it is often found as a multifocal mass with dynamic changes in signs and symptoms.[1,3] Clinical presentations vary from asymptomatic cases to highly unstable patients, depending on the tumor’s size and location. Such tumors are typically fast-growing with a high potential for deep cardiac invasion. Tumor-induced obstruction of cardiac flow may result in syncope, cardiac arrest, arrhythmias, or embolic events.[5] Thus, CMMM should be considered a potentially dangerous but treatable condition.
Historically, CMMM was an incidental autopsy finding in 47%-64% of patients with melanoma postmortem.[1,2] In most cases, CMMM was clinically silent with unclear medical significance, and its clinical importance may be underestimated.
CMMM can theoretically arise from any primary melanoma site or from endocardial or myocardial tissue. Histological confirmation is essential but challenging in living patients. Percutaneous heart biopsies are difficult, so CMMM is easier and safer to confirm through surgical excision during open heart surgery. Histological proof of atypical melanocytes and dense intracytoplasmic melanin pigment is critical to confirm the diagnosis.[1,6,7]
Today, thanks to advances in echocardiography, CMMM is relatively easy to detect. It is often misdiagnosed as valve vegetation or another type of mass due to similar echocardiographic appearances. TEE is considered the optimal imaging technique for CMMM, while cardiac catheterization, CT, or MRI may be used to assess associated cardiac malformations and tumor involvement. A PET scan is mandatory to locate the primary melanoma.[1,3]
There is no standardized treatment for CMMM. Urgent surgical excision should be performed as early as possible, particularly in symptomatic cases. In our case, we approached the tumor via the right atrium, which allowed for a clear, sharp excision while preserving the tricuspid valve and right atrium. A thrombus on the tumor surface is an important finding, supporting the theory that recurrent embolization could result from CMMM embolization and secondary endothelial damage with thrombosis.
CMMM carries a poor prognosis due to extensive intracardiac infiltration and/or non-cardiac metastasis.[2] Standard chemotherapy has yielded 5-year survival rates of 5%-10%, but outcomes have improved since the introduction of immunotherapies in 2011.[2,4,5]
A potential limitation of this case presentation could be the lack of long-term follow-up data. Although the patient was reported to be symptom-free and well 6 months after surgery, malignant melanoma is known for its high recurrence rate, even decades after initial diagnosis. Without extended follow-up over several years, it is difficult to assess the long-term outcomes of the patient, including the possibility of recurrence, metastasis, or late complications from both the melanoma and the surgical intervention.
Additionally, another limitation could be the absence of detailed information on the patient’s post-surgical treatment plan, including specific immunotherapies or chemotherapies used, and their efficacy over time. This would provide valuable insight into how current therapies influence survival rates and recurrence in patients with CMMM.
CONCLUSION
In conclusion, we report a rare case of CMMM causing right atrial obstruction 16 years after the primary presentation. Urgent surgical excision resulted in a favorable outcome. The patient survived the operation, was referred for further oncologic treatment, and remained well without recurrence 6 months post-surgery. This case highlights the high recurrence rate of malignant melanoma, even decades after initial diagnosis, and underscores the importance of lifelong follow-up
Cite this article:
Jonjev ZS, Samardžija G, Todić M, Rajić J, Majdevac S, Kalinić N. Surgical Treatment of Right Atrial Metastasis of the Malignant Melanoma: A Case Report. Journal of BUON. 2024;27:28-35.
ACKNOWLEDGEMENT
None.
ABBREVIATIONS
| CMMM | Cardiac Metastasis of Malignant Melanoma |
|---|---|
| CT | Computed Tomography |
| EF | Ejection Fraction |
| HR | Heart Rate |
| MRI | Magnetic Resonance Imaging |
| PET | Positron Emission Tomography |
| RA | Right Atrium |
| RV | Right Ventricle |
| TEE | Transesophageal Echocardiography. |
References
- Onan B., Onan I. S., Polat B.. Surgical resection of solitary metastasis of malignant melanoma to the right atrium.. Tex Heart Inst J.. 2010;37:598-601. [Google Scholar]
- Poulsen C. B., Weile K. S., Schmidt H., Poulsen S. H.. A case report: metastasis of melanoma to the heart in an era of immunotherapy.. Eur Heart J Case Rep.. 2019;3:1-7. [Google Scholar]
- Judge J.M., Tillou J.D., Slingluff C.L., Kern I.L., Kron I.L., Weiss G.R., et al. Surgical management of the patient with metastatic melanoma to the heart.. J Card Surg.. 2013;28:124-8. [Google Scholar]
- Márquez-Rodas I., Muñoz Couselo E., Rodríguez Moreno J.F., Arance Fernández A.M., Berciano Guerrero MÁ, Campos Balea B, et al. SEOM-GEM clinical guidelines for cutaneous melanoma (2023).. Clin Transl Oncol.. 2024;26(11):2841-55. [Google Scholar]
- Abohelwa M., Elmassry M., Del-Rio-Pertuz G., Wischmeyer J.. Atrial Flutter Leads to Diagnosis of Metastatic Melanoma Involving the Heart.. Tex Heart Inst J.. 2023;1:e217709 [Google Scholar]
- Hopkins N. S., Laplant J. F., Randall M. B., Wilson M. W.. Metastasis of Conjunctival Melanoma to the Cardiac Atrium: A Case Report.. Ophthalmic Plast Reconstr Surg.. 2023;39:e104-7. [Google Scholar]
- Avranas K, Eisenbach C, Flechtenmacher C, Korosoglou G.. Diagnostic Pathway From Incidental Mass to Metastatic Melanoma: Role of Multimodal Imaging and Medical Therapy. A Case Rep.. JACC. 2024;29(1):102146 [Google Scholar]